Changing Haemophilia: Symptoms, types and causes
Are you looking to learn the basics about haemophilia types, symptoms and genetics? Then read on for an overview of the rare disease.
This is general disease awareness and should not be understood as medical advice. If you experience symptoms of COVID-19 or have questions, doubts or concerns, you should contact your doctor. Always follow the advice of local authorities.
Haemophilia is a genetic disorder in which the blood doesn’t clot normally. Perhaps the most well-known “bleeding disorder”, haemophilia can be mild, moderate or severe depending on the amount of so-called “clotting factors” – a group of proteins – in the blood. Haemophilia is a world-wide issue which occurs in all racial groups, but almost exclusively affects men.
Haemophilia is a rare condition. The most common type of haemophilia affects approximately 1 man out of 5 thousand, whereas only 1 in 25 million women is living with haemophilia. The global incidence of hemophilia is not precisely known, but it is estimated that 1,125,000 people live with haemophilia. In other words, roughly 0.02% of the world’s population is affected.
Why should blood clot in the first place? To stop bleeding, simply, whether the bleeding happens internally or externally. The clotting of normal blood is due to the action of a group of proteins called “clotting factors”. A haemophilia patient’s blood, however, contains less than the normal amount of some clotting factor.
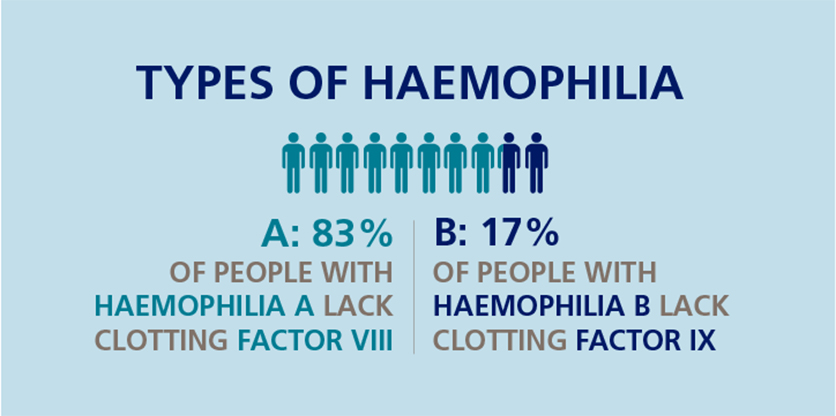
While all people living with haemophilia experience the same main symptom – prolonged and frequent bleeding – patients differ with respect to which clotting factor they need. The name of the diagnosis varies accordingly:
- Haemophilia A or “classic haemophilia” is the most common type of the disease. It is caused by having reduced levels of clotting factor VIII (FVIII).
- Haemophilia B, also known as Christmas Disease, is caused by having reduced levels of clotting factor IX (FIX).
Symptoms
The precise symptoms of haemophilia vary according to the degree of clotting factor deficiency. The normal range of FVIII or FIX level is between 50-150%.
Here is a breakdown of the three relevant categories:
- Mild haemophilia
Mild haemophilia may not cause any symptoms at all until an irregular event gives it away – for example, a serious wound or an invasive dental procedure. In the blood of people with mild type A or B haemophilia, the amount of factor is 6–50%.
- Moderate haemophilia
People with moderate haemophilia tend to bruise easily and may experience internal bleeding around joints. Familiar to the majority of people with haemophilia, the experience of a so-called joint bleed can range from slight irritation to swelling, stiffness, warmth and severe joint pain, especially if not treated. In the blood of people with moderate type A or B haemophilia, the amount of factor is 1–5%.
- Severe haemophilia
For those with severe haemophilia, bleeding occurs spontaneously, which is to say “for no apparent reason”. The bleeding may occur from or in the nose, gums, joints or muscles. Bleeds inside the skull (intracranial hemorrhage) are a rare and almost never spontaneous occurrence in an estimated 3% of people with severe haemophilia. In the blood of people with severe type A or B haemophilia, the amount of factor VIII or IX is less than 1%. Severe haemophilia affects approximately 37% of all men who live with haemophilia.
No matter the severity of the condition, symptoms rarely appear within the first 9 months of a person’s life.
Inheriting haemophilia
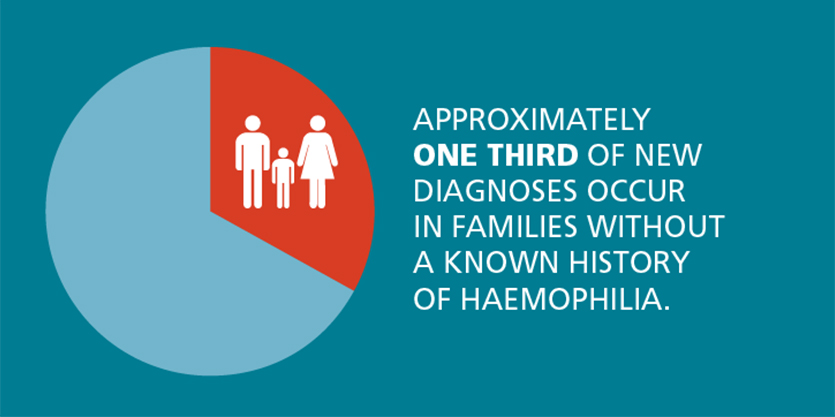
As mentioned above, haemophilia is a genetic disorder. The genetic alteration that results in a lower amount of clotting factor is located on the X chromosome and passed on from mother to child, which makes the disorder hereditary. Approximately one third of new diagnoses, however, occur in families without a known history of haemophilia.
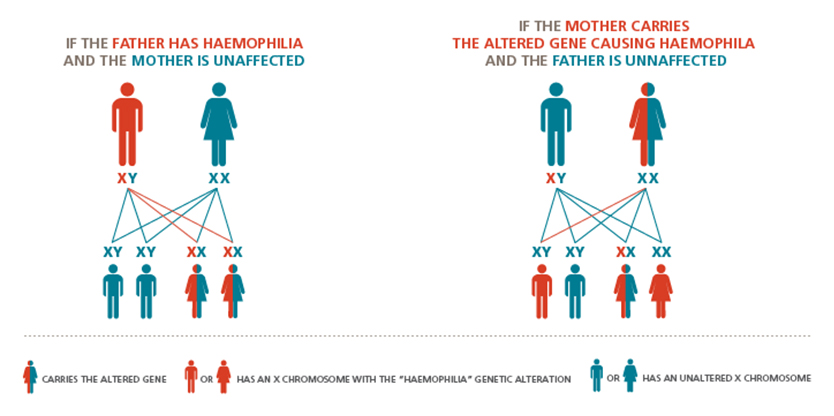
Both men and women have an X chromosome, but whereas women have two, men have only one X chromosome. This is the reason why women can be carriers of the so-called haemophilia gene (without having the disorder themselves) and pass it on to their sons or daughters. Sons and daughters who inherit the affected X chromosome will have haemophilia or be a carrier, respectively, since males do not have a spare chromosome.
Suppose a man without the haemophilia gene decides to have a child with a woman who carries the gene. Their child will not necessarily have haemophilia. The same is true for a woman who does not carry the haemophilia gene and has a child with a man who has haemophilia – their child will not necessarily have haemophilia.
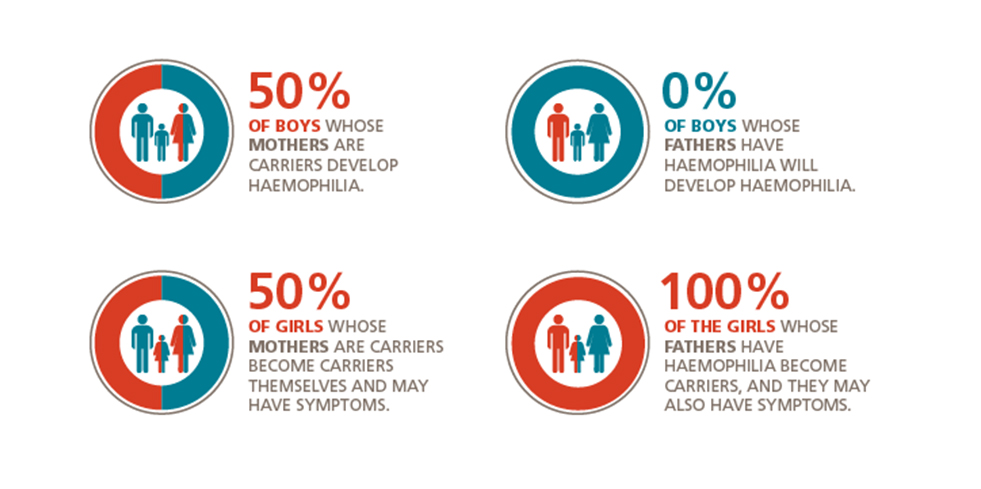
Here is another way of representing the susceptibility to haemophilia characterising the next generation:
- 50% of boys whose mothers are carriers develop haemophilia.
- 50% of girls whose mothers are carriers become carriers themselves and may have symptoms.
- None of the boys whose fathers have haemophilia will develop.
- All of the girls whose fathers have haemophilia become carriers, and they may also have symptoms.
The future of haemophilia

While there is currently no cure for haemophilia, the quality of care and treatment has improved considerably over the last several decades. Despite the fact that no two conditions are identical, the vast majority of haemophilia patients with access to healthcare can live fulfilling and active lives.
