Being an advocate in the haemophilia community, I’m always the first to say that no question is a silly question. When haemophilia is always on your agenda, it’s easy to forget just how rare of a condition it is and that most people won’t have heard of it. With this lack of awareness comes misconceptions. In my 27 years of living with haemophilia I feel like I’ve heard everything when it comes to people’s misconceptions of the condition (some more ridiculous than others) and correcting these is often part and parcel of being an advocate. So, I’m here to set the record straight on some of the big misconceptions I’ve heard over the years.

“If you get a cut, will you die?”
If I had a pound for every time I got asked this one!... This was something asked more when I was younger. Possibly something to do with the morbid curiosity of children. As ridiculous of a question it may sound, I can see why people’s minds go there. I tell them that my haemophilia means my blood doesn’t clot properly, so it is harder for me to stop bleeding. Most people then picture an everyday cut or scrape. They then assume things like this are extremely dangerous or life-threatening for me. So will I die from a paper cut?... No. Thankfully! Due to my lack of skills in the kitchen I’ve cut myself an embarrassing number of times with sharp knives. Not pleasant… but not life-threatening! Most minor cuts and scrapes can be treated with basic first aid.
Most problematic bleeding people with haemophilia experience are internal bleeds into the joints and muscles. These can be very painful and debilitating. Plenty of treatment and rest is required to recover. Repeated bleeding into a joint can cause long-term joint damage, so we want to avoid these bleeds. Also, people with haemophilia need to be very careful when it comes to head trauma. The risk of bleeding into the brain is serious for anyone, let alone someone with a bleeding disorder.
“Haemophilia is a problem with your platelets, right?”
I think this misconception comes from basic biology lessons at school. We learn that platelets are an important cell in the blood that helps us to clot and form scabs for example. So, it’s understandable people think haemophilia is where my platelets don’t work or I don’t have enough (these conditions do exist…they just aren’t called ‘haemophilia’).
For your platelets to stick together and form a strong and stable clot, something called the “coagulation cascade” must occur. Don’t worry, I won’t bore you with the details! However, this process involves proteins called clotting factors. People with haemophilia don’t have as many clotting factors in their blood. People with haemophilia A are deficient in Factor VIII and people with haemophilia B (the type I have) are deficient in Factor IX.
The truth is that my platelets are perfectly fine! I just don’t make enough Factor IX… that’s kind of catchy!

“Haven’t they cured haemophilia?”
Growing up, a simple “no” was often the answer. I was aware that researchers were working on gene therapy treatments with the goal of curing haemophilia, but there was still a long way to go. However, scientific advances have made answering this question a bit more complicated. At present there isn’t officially an approved and recognised cure for haemophilia. Even the interpretation of the word “cure” is something that’s discussed and debated within the community. It means something different to different people. In clinical trials some people’s factor levels have reached the normal range (>40%), some have reached the moderate to mild range (2-40%). We have seen a lot of variation. Studies are still ongoing, and many questions remain.
My short answer to this question at present is “not yet!” because I believe we will get there. I hope to see a cure within my lifetime.

“How come only men get haemophilia?”
Newsflash… they don’t! Women can in fact have haemophilia. Granted, it’s rarer for women to have severe haemophilia (factor level <1%) but it can happen. However, excellent advocacy work within the haemophilia community has highlighted the challenges women face. It’s common knowledge that women can be “carriers” of haemophilia; mothers have a 50% chance of passing the faulty gene to their sons, who will have haemophilia. It has been found that carrying the faulty haemophilia gene can also result in lower factor levels in some women… factor levels in a range we’d consider to be mild or moderate haemophilia in men… so why shouldn’t the same classification apply to women?! Thankfully this is starting to be recognised within the medical world, meaning women with haemophilia should have equal access to treatment and care. However, we need to continue raising awareness about this issue.
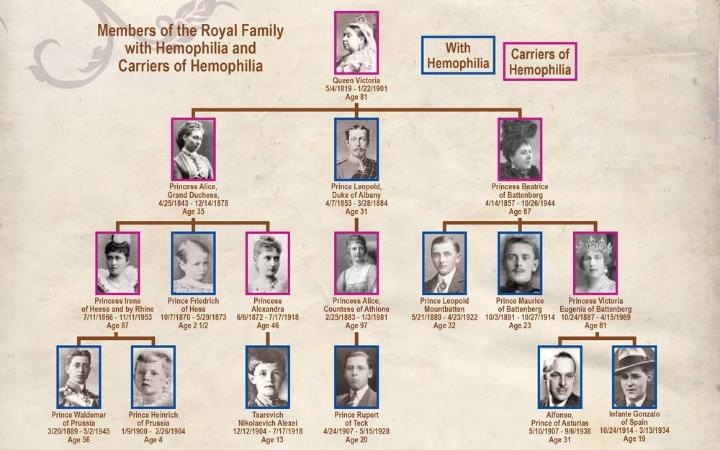
“Does that mean you’ve got royal blood?”
Whilst Prince Pembroke does have a nice ring to it, I am not related to royalty. Many have heard that Queen Victoria was a carrier of haemophilia, specifically B. This resulted in the condition affecting many European royal families in the 1800s.